Introduction
The concept of epidemiological transition of mortality and cause of death dates back to the neolithic age. Omran in 1971 divided the manifestation of the phenomena into three phases. The first phase of The Age of Pestilence and Famine is characterized by an increase in infectious diseases, malnutrition and high mortality. This is followed by The Age of Receding Pandemics distinguished by progressive decrease in frequency epidemic peaks, declines in mortality rates, and increased life expectancy. The third and most relevant phase is The Age of Degenerative and Man-Made Diseases marked by continued increase in life expectancy and decline in mortality rates. Most developing countries, including Kenya, are in this third phase. This phase is associated with mortality increased mortality, and a shift from infectious diseases/communicable diseases to non-communicable diseases (NCDs).
According to the World Health Organization Global Status Report on NCDs, the number of deaths is projected to increase from 38 million in 2012 to 52 million by 2030. 48 per cent of these deaths are expected to occur in low- and middle-income countries. In addition, 42 per cent of NCD-related deaths occur before the average age of death of certain populations, otherwise known as premature mortality. In Kenya, NCDs accounted for 27.1 per cent of deaths in 2016, which was an increase from 15.8 per cent in 2000. The nature and severity of NCDs have added onto the burden of the unfinished agenda on infectious diseases in developing countries, resulting in a duo-disease burden.
The importance of NCDs as a health issue has been recognized and resulted in various global declarations and conventions including the Brazzaville Declaration on non-communicable diseases prevention and control in the WHO African Region (2011) and the UN Global Action Plan for Prevention and Control of NCDs 2013-2020. Their continued prevalence also resulted in their inclusion in the UN Agenda 2030, AU Agenda 2063, and EAC Agenda 2050. The Kenya Vision 2030 and subsequent Medium-Term Plans (MTPs) also make provisions for NCD control and prevention. Under MTP III, the government seeks to estimate the NCD burden and develop a mechanism for long term financing of NCDs.
Cancer as a Non-Communicable Disease
Cancer, which is the abnormal, invasive, uncontrolled growth of cells, is among the top four (4) leading causes of death among NCDs (alongside cardiovascular diseases, respiratory diseases and diabetes). The global incidence of cancer rose to 18.1 million new cases whereas the number of deaths associated with cancer increased from 9 million in 2016 to 9.6 million in 2018. Its causes have been categorized into modifiable and non-modifiable factors. Modifiable factors are behaviours and exposures that can raise or lower a person’s risk of cancer. They are further divided into behavioural risk factors such as diet, smoking, or drinking alcohol and environmental risk factors such as ultraviolent radiation. Non-modifiable risk factors mainly include biological risk factors such as genetic predisposition, sex, and aging. Cancer prevention strategies mainly focus on reducing exposure to modifiable risk factors. The focus on non-modifiable factors mainly revolves around early detection.
Status of Cancer in Kenya
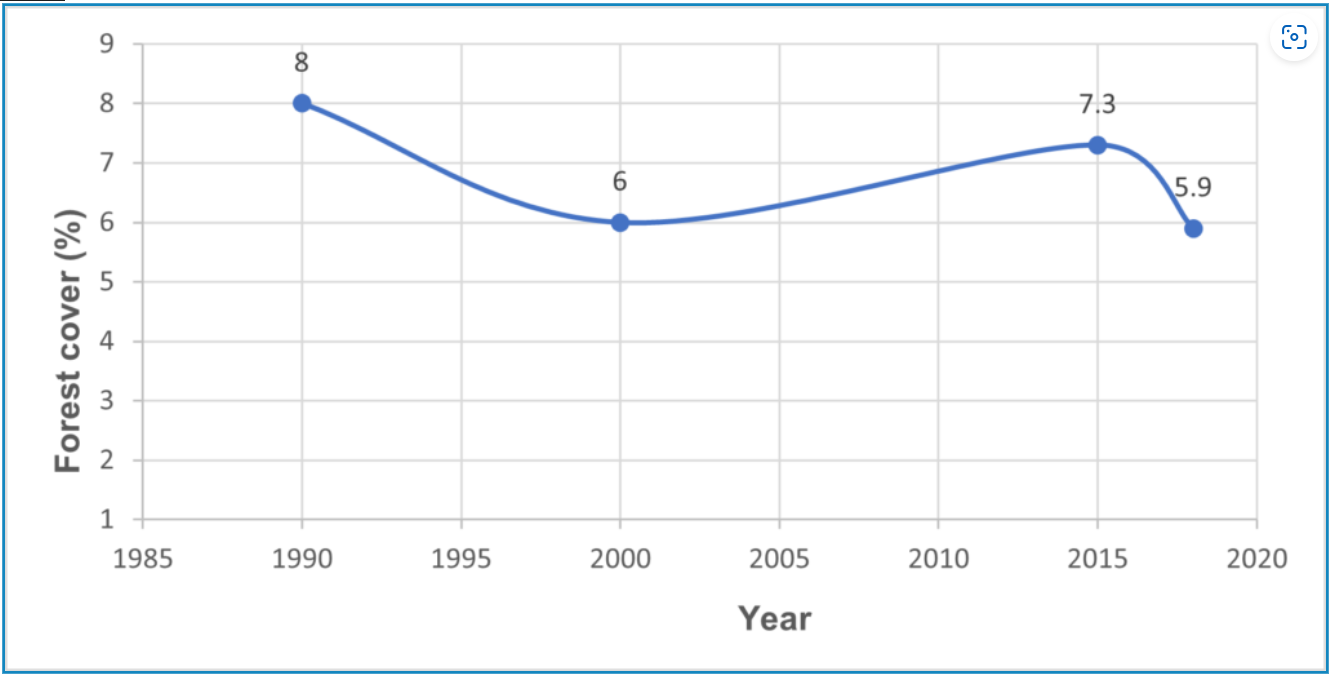
Cancer accounted for 9 per cent of all deaths in 2017, representing a growth of 41 per cent between 2010 and 2017. It has been ranked third amongst the leading causes of death (after Malaria and Pneumonia) and first amongst the NCDs since 2011.

Newly reported cancer cases were 47,887 in 2018. The disease is observed to affect more women than men. In 2018, 60 per cent of the newly reported cases and 57 per cent of the registered cancer related deaths were female. According to the Global Cancer Observatory in 2018, breast, cervical, and esophageal are the leading cancers affecting women and they affect 20.9 per cent, 18.3 per cent and 7 per cent of women in the population, respectively. Esophageal, prostate and colorectum cancers were the most common cancers amongst men with incidence rates of 14.9 per cent, 12.4 per cent, and 5.9 per cent, respectively. Kaposi sarcoma was previously the third most prevalent cancer among men. Among children, retinoblastoma, nephroblastoma, burkitt’s lymphoma and acute lymphoblastic lymphoma were cited as the most common. The risk of developing cancer before the age of 75 is 18 per cent while the risk of dying from cancer before the age of 75 is 14 per cent.
Effects of Cancer
The burden of cancer is felt both at national and household level. At the national level, cancer prevalence impedes poverty reduction initiatives due to factors such as loss of a productive population resulting from premature mortality and loss of productive time due to care giving. In addition, increased incidence of cancer has resulted in an increase in government expenditure on treatment and palliative care evidenced by, among other factors, an 11 per cent growth in National Hospital Insurance Fund (NHIF) expenditure on cancer treatment in 2018/19.
At household level, enhanced technology that allows for outpatient care has led to an increase in reliance on informal care giving. Informal care givers often leave their jobs entirely or significantly reduce their number of hours of work, thus resulting in loss of household income. In addition, the financial burden posed by the high cost of drugs and treatment is heightened by costs outside the health system such as dietary requirements. Persistence of financial burden increases vulnerability to poverty through loss of savings and debt accumulation. The pressure related to care giving has also often been linked to both physical (cardiovascular diseases) and psychological (anxiety and depression) health implications. Nonetheless, research has found that that patients cared for by a caregiver are less symptomatic and experience better physical and mental health outcomes.
Legal Framework
In a bid to reduce the long-term disease burden of cancer, the government has put in place various policies, strategies and legislative frameworks to mainstream the coordination of interventions associated with cancer treatment and control. For instance, the basic law governing creation of awareness, early detection and treatment is the Cancer Control Act, 2012. Under Section 26, the Act bars exclusion from credit or insurance services and states that a person shall not be compelled to undergo screening or disclose their cancer status for the purpose of obtaining the same. The Act further stipulates under Section 27 that a person with cancer or perceived to have cancer shall not be denied health services in any institution or charged a higher rate. The Act also puts in place frameworks for establishment of the National Cancer Institute whose mandate is to come up with overall national agenda for the treatment and management of cancer country wide. Amendments to the Cancer Control Act, 2012 to provide for additional functions of the county governments and commitments made under the UN Global Action Plan for Prevention and Control of NCDs (2013-2020) are underway. This is expected to resolve challenges linked to coordination of national and county governments in cancer control.
Government and Non-State Actor Initiatives
The Act is complemented by the Ministry of Health’s 5-year National Cancer Control Strategies, the most recent covering the duration 2017-2022. In line with implementation of the strategy, a country-wide free cancer (breast, cervical, and prostate) screening programme has been launched and is in the process of being rolled out. So far, it has been rolled out in Kakamega, Kisumu and Embu counties.
Kenya also commemorates World Cancer Day by creating awareness on the importance of cancer screening for early detection. Cancer chemotherapy centres have also been established in counties such as Bomet and Nyeri. NHIF, which is the social insurer of the government, also covers cancer under the following benefit packages: Oncology cover which caters for radiotherapy sessions, basic and complex chemotherapy; surgical cover which covers minor surgeries such as lumpectomies, major surgeries such as mastectomies and specialized surgeries such as mammectomies; radiological cover which covers ultra sounds, CT scans, MRIs, and pet scans; in-patient cover which covers bed charges; and foreign treatment cover.
The government is also putting in place measures to enhance monitoring and evaluation of cancer incidence. These include developing standardized cancer risk indicators, linking data collection to health management information systems, integrating cancer indicators into existing data collection tools (STEPS Survey and Kenya Demographic and Heath Survey), and enhancing existing cancer registries. More recently, the government has rolled out Universal Health Coverage, which has a component of preventative care, in four counties (Nyeri, Machakos, Kisumu and Isiolo) to further reduce vulnerability to poverty caused by out of pocket expenditure on health care.
Other non-state actors such as the private sector and non-governmental organizations also play a critical role in the fight against cancer. For example, most hospice care and palliative care clinics for cancer patients are private entities. These, however, tend to be unaffordable for low income households and hence further contribute to the influx in the number of informal care givers. Various private hospitals have also established comprehensive cancer units to complement existing government facilities in the provision of cancer services. Insurance companies such as ICEA Lion have also developed cancer packages to reduce vulnerability of families to financial hardship associated with cancer treatment. Non-governmental organizations, such as the Beth Mugo Cancer Foundation (BMCF), and World Health Organization, among others, have also undertaken to promote the uptake of cancer screening aimed at enhancing prevention and early detection of cancer.
This notwithstanding, one of the major challenges affecting the quality delivery of cancer-related health services in the country is inadequate health workforce for cancer prevention, detection and treatment. Currently, there are 35 oncologists against a population of 47.8 million people. As such there is limited capacity for the health sector to handle the complex nature of cancer.
Conclusion
Cancer is a major threat to sustainable development as the associated disease burden is expected to continue increasing for the foreseeable future. In particular, premature mortality and lost productive life have an enormous impact on the economic growth of a country. Cancer also disproportionately affects women, men and children and further impede poverty reduction efforts. The government and non-state actors have put in place various initiatives targeting different age-groups in the population. These efforts have resulted in remarkable progress in the fight against cancer, albeit rather slowly due to existing systemic and structural challenges.
One of the major challenges facing cancer control is the ill-preparedness of the health workforce for cancer prevention, detection and treatment. There is need for recruitment of additional cancer specialists and investment in the development of new options for both the education and in-service training of health care workers to enhance preparedness of the health workforce in the fight against cancer. In addition, there has been an upsurge in informal care-giving coupled by evidence revealing its importance. Borrowing from the experience of the United States, there is need to put in place evidence-based legislative actions to tackle financial security and workplace challenges, among other risks caregivers are exposed to. Finally, all cancer control strategies should be coupled with adequate investment to obtain better outcomes.
By Samantha Luseno and Lawrence Njoroge